Could a single synthetic molecule outsmart a variety of drug-resistant bacteria?

An estimated 2.8 million people in the U.S. contract infections each year from bacteria resistant to antibiotics, according to the U.S. Centers for Disease Control. More than 35,000 of them die.
Despite the mounting toll — and the prospect of an eventual surge in superbug fatalities — the development of new antibiotics has failed to keep pace with the threat. A new medicine capable of combating Gram-negative bacteria, a particularly hardy type of bug with inner and outer membranes that antibiotics struggle to cross, hasn’t hit the market in 50 years.
So when a new substance appears on the scene with a decent chance of eventually becoming one of these desperately-needed drugs, scientists say it’s a big deal.
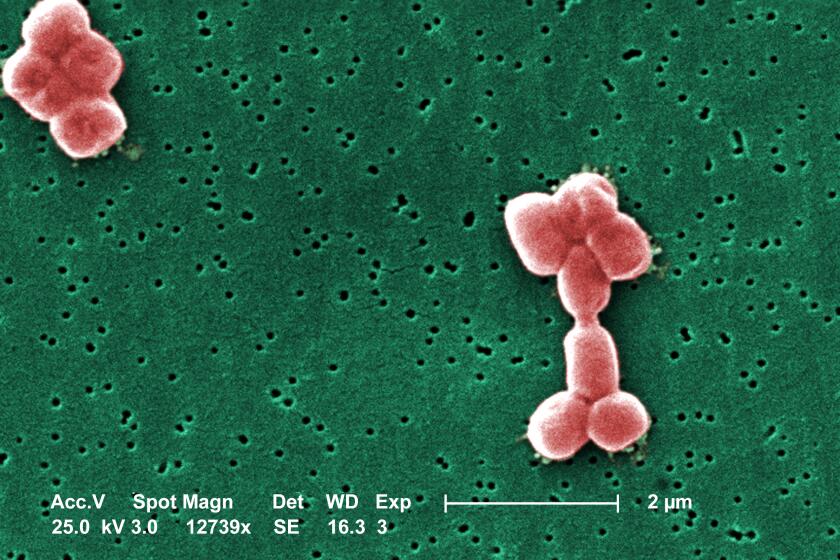
Researchers at Harvard and the University of Illinois at Chicago have created a new molecule that effectively vanquished multiple types of bacteria when tested in animals. The organisms on its hit list included strains of Staphylococcus aureus, Escherichia coli and other pathogens that have become resistant to most antibiotics currently available.
The new molecule, dubbed cresomycin, was described Thursday in the journal Science.
Cresomycin is not yet a drug, nor is it close to being ready for clinical trials in humans. But it represents a promising enough step toward new treatments that a nonprofit dedicated to fighting superbugs gave its Harvard creator $1.2 million this week to develop cresomycin and similar substances into new oral antibiotics.
“I’ve never been more optimistic or excited about a project,” said Andrew Myers, the Harvard University chemist whose lab developed the molecule.
For the first time in half a century, researchers have identified a new antibiotic that appears to kill a deadly, drug-resistant superbug.
Cresomycin belongs to a class of antibiotics known as enhanced lincosamides. It works by targeting a bacterium’s ribosome, the tiny protein factory tucked in every living cell.
“Ribosomes can be viewed as a molecular 3-D printer,” said Yury Polikanov, a structural biologist at the University of Illinois at Chicago and a co-author of the paper.
Just as those machines take plastic molecules and use them to construct objects of any shape, ribosomes take genetic information from RNA and use it to crank out proteins.
Since proteins are essential to virtually all cellular activity, ribosomes are vital to bacteria. That’s why many antibiotics are designed to target them.
But bacteria are always evolving — and embracing new adaptations that help them thwart our attempts to kill them. In some cases, bacteria do this by inserting a tiny chemical dab known as a methyl group into its ribosome. When an antibiotic attempts to bind to the ribosome, that methyl group repels it.
The methyl group acts like a tiny thumbtack set out on the seat the antibiotic was hoping to take, Polikanov said.
“Not very comfortable to sit when a needle is poking you,” he said.
But unlike previous antibiotics, cresomycin binds so tightly to the ribosome that it essentially negates the effect of the methyl group.
Returning to the thumbtack analogy, Polikanov said the molecule sits on its ribosome seat with such force that it drives the tack into the chair. The ribosome’s best defense is neutralized, allowing cresomycin to get on with its bacteria-killing work.
Using soil from a grassy field in Maine and a miniaturized diffusion chamber, scientists have cultivated a microbe that could help tame the spread of antibiotic-resistant superbugs.
In test tubes, cresomycin proved much more effective than currently available antibiotics at inhibiting the growth of several types of bacteria. These included a nasty bug called carbapenem-resistant Acinetobacter baumannii that tends to show up in hospitals, E. coli and Neisseria gonorrhoeae, the bacteria that causes gonorrhea.
Researchers then took 20 mice and deliberately infected them with methicillin-resistant S. aureus, better known as MRSA. Half the mice were given four injections of cresomycin over the course of a day, and the other half received injections without the active ingredient.
All but one of the mice who didn’t get treatment were dead two days later. In contrast, all 10 of the mice who received cresomycin were still alive seven days after treatment.
In the Science paper, the authors were quick to note that cresomycin is not yet ready for clinical trials in humans.
The Harvard lab manufactured more than 60 molecules in its quest for one as effective as cresomycin, and that presents just a tiny fraction of the “exponentially greater numbers” of possible variations they could make, Myers said. As the researchers continue their work, they may find an even better candidate for eventual drug development.
Yet even at this stage, cresomycin represents an exciting possibility, according to experts who weren’t involved in the work.
“Probably about one in 1,000 projects make it to the level where he’s got it,” said Richard Alm, chief scientific officer at the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator, or CARB-X, which gave Myers the $1.2-million grant. Of potential drugs that make it to the stage of development that cresomycin has reached, Alm estimated that one in every 30 or 40 ultimately has enough positive data to win approval from the U.S. Food and Drug Administration.
An elderly man in Alaska has become the country’s first person confirmed to have died of Alaskapox. Here’s what you should know about the disease.
CARB-X is a global nonprofit dedicated to speeding up development of new antibiotics. It has made nearly 100 grants so far to companies or academic institutions working to treat, prevent or diagnose antibiotic-resistant infections. Headquartered at Boston University, the accelerator is funded by the governments of the U.S., the United Kingdom, Canada and Germany, as well as the Bill and Melinda Gates Foundation, Wellcome Trust and the Novo Nordisk Foundation.
Development of antibiotics has stalled in part because they aren’t as potentially lucrative as other drugs, Alm said. They aren’t meant to be taken over the long term like medications for chronic conditions like diabetes or high blood pressure. And doctors want to use the most potent ones as rarely as possible, to give bacteria fewer chances to develop resistance to them.
All of that makes it a lot harder to recoup the costs of producing an effective antibiotic, Alm said. Efforts like CARB-X are an attempt to keep the pipeline from drying up.
“If your house is burning, you don’t have time to buy a fire truck, hire firemen and train them to come and put your fire out. You need them ready to go,” Alm said. “That’s the same with antibiotics. If you go into hospital and you get a superbug, you need an antibiotic that is there on the shelf.”